Learning to Identify, Label, and Communicate Needs
Posted by Kim Clairy OTR/L on Apr 7th 2021
 Diagnosed with Autism as an adult and suffering from a severe eating disorder (ED) for over a decade I broke through many barriers. Over the years I developed strategies to help me function.
Diagnosed with Autism as an adult and suffering from a severe eating disorder (ED) for over a decade I broke through many barriers. Over the years I developed strategies to help me function.
The top three things I had to learn before successfully implementing strategies for problematic behaviors were: First- identify my body signals and what they meant (AKA interoceptive awareness); Next- label the signals with the associated feeling word; Then- find a way to communicate feelings and needs to others in a way they can understand. Here is part of my story and my top three things to learn.
Part of My Story
In me contained all the ingredients for a perfect storm; just waiting to erupt. At age 19 it made landfall. This is when I developed an eating disorder. I received intense therapy the first few years of the disease; however, I became what they call a “frequent flyer” and “treatment resistant.”
At age 29 I was told “your Autism is severe, you need to live in a nursing home.” The following year I was told “You need hospice.” I knew this was not my fate; I just needed to figure out how to cope with my disordered behaviors that were exasperated by my Autism traits. Determined, I put to use my skills as an occupational therapist along with my super Autism abilities for intense hyper-focus, detailed thinking, finding patterns, and solving complex problems.
Early in my eating disorder, I recognized many eating disordered behaviors were compounded by, or the result of, Autism traits. I developed my own problem-solving method and eventually learned to distinguish between ED symptoms and behaviors stemming from Autism. I thought figuring out the etiology to my behaviors would lead to recovery; if I understood the reason behind the problem, I could then fix it. I was wrong.
Realizing this, I tried sharing my insights and ideas with providers for years. I had very little success as I was unable to communicate in their language, and they were unable to understand mine. Despite the false labels and accusations of being defiant or manipulative, I persisted.
With the help of one nurse, at the age of 26 I learned how to recognize and label my emotions with a feeling word. Before this, I did not know what frustrated or overstimulated felt like, or rather I did not know the word for what I was experiencing. By this point I had spent year in therapy. Years where I was being taught what to do when I felt overstimulated, frustrated, anxious, or angry. Years where this information went in one ear and out the other.
You see, how I experience emotions is different. I experience them through color, temperature, and texture. When overstimulated I sense neon yellow electricity shooting from my body. Frustration looks like brown dots that are damp and swirling. I received blank looks when sharing these feelings. If a therapist was trying to teach emotional coping skills, I did not understand what the feeling words referred to. I had no idea what overstimulated, or frustration meant. Not until that one nurse when I was 26.
Feelings Person
Here is how it worked
- Nurse A drew a very large stick figure on a sheet of paper
- She would then tell me a feeling, give an example of when she felt that way, and say where and how she felt it in her body
- Next she chose a color and shaded in where she felt the feeling on the diagram.
- Then she asked me for a time when I felt that emotion. If I was unable to identify a time she would tell me of a time she witnessed me feeling the emotion.
- I was asked to describe how my body felt during that emotion (what sensations & where).
- Lastly, I chose a color and shape for the emotion and shaded it in on the diagram.
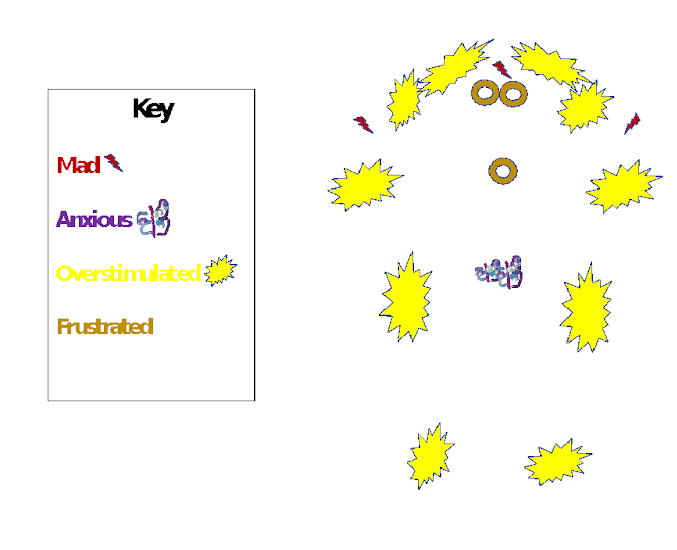
We did this with 12 emotions; it became my feelings reference when I was unsure of my emotions. Below is an abbreviated example.
After learning to identify my body signals and its associated feeling word I was better able to learn coping strategies for problematic behaviors. While I did learn great coping skills, I was unable to implement them independently at first because of challenges with executive functioning and sensory processing. I needed help from others but was unable to effectively communicate my feelings or needs to receive the help. This became my next problem to solve. Below are descriptions of a few tools I developed to help with communicating my feelings.
Feelings Log
Nurse A taught me my behaviors/reactions are inconsistent with what others recognize as a particular feeling which then led to misunderstandings. Together, we created a feelings log- an invaluable reference and decoder to my emotions. It helped them to better identify what I am feeling based on what I am doing and provided guidance on how to help. I shared this tool with my now husband on our 3rd date. He believes “all women should come with a feeling manual!”
Feelings Blocks
My blocks, a visual tool, helped me as I was learning to pair my feelings with coping strategies. I also used them to communicate where I was if I had gone missing, which reduced the worry that often resulted when I “disappeared” (to cope with a feeling). They are a great tool because they are tactile, visual, can be manipulated, limit the number of coping choices, provide a reference to feelings, and don’t require talking to use. Plus, they are homemade!
Ten Point Scale
This is a 1-10 scale of emotional and sensory regulation states that my husband and I developed together. It further developed my interoceptive awareness, helps with self-regulation, communicates levels of regulation to others, and helps others know when I am in need of assistance. This tool allows me to communicate my needs even when I am unable to speak.
Final Thoughts
The top three things I had to learn (identifying body signals and what they mean, labeling signals with the associated word, and finding a way to effectively communicate my feelings and needs to others) before successfully implementing strategies for problematic behaviors were the building blocks to replacing negative behaviors with positive ones. They built a foundation for my eating disorder recovery and for my ability to manage Autism challenges. They made it possible for me to develop relationships, carry out daily tasks, travel the country educating others on Autism, and prove that I did not need hospice to live in a nursing home.
Kim Clairy OTR/L is an occupational therapist, public speaker, autism advocate, and private consultant. To read Kim's blog or contact her for a speaking engagement please visit her website KimClairy.com







